Acquired epilepsy is a neurological disease with a chronic course; it is characterized by the presence of repeated seizures due to excessive electrical activity of nerve cells in the brain. This type of paroxysm accounts for 25% of cases.
Symptoms of the disease are as follows: short-term memory loss, uttering inarticulate sounds, automatic actions, convulsive muscle twitching. With a long course of the disease, patients experience personality disorders: increased sentimentality, suspicion, cruelty, outbursts of anger, and a tendency to take revenge. Speech is stereotyped and slow; such people cannot quickly switch from one topic to another.
This type of disorder is always secondary; most often the causes of focal epilepsy are associated with:
- metabolic abnormalities;
- abnormal changes in blood vessels;
- volumetric processes in the cerebral cortex;
- congenital developmental defects;
- head injuries;
- infectious lesions;
- poisoning;
- hypoxia.
The acquired variety is diagnosed using instrumental and laboratory studies. The fundamental method for determining the focus of paroxysmal activity is computer imaging - MRI or CT.
Treatment is aimed at eliminating the cause of the abnormality, reducing or eliminating seizure activity, improving quality of life and preventing disability. Therapy includes taking medications or undergoing surgery.
Causes of epilepsy
Such genetic defects do not develop out of nowhere: they are provoked by the following factors:
- hypoxia during pregnancy;
- infections in the prenatal period (rubella, toxoplasmosis, herpes infection, etc.);
- birth injury.
- underdevelopment of individual brain structures acquired during the prenatal period, not considered within the framework of idiopathic epilepsy;
- traumatic brain injuries;
- neoplasms in the brain;
- chronic alcoholism and drug addiction;
- infectious damage to the central nervous system (meningitis, encephalitis);
- side effects of certain drugs (neuroleptics, antidepressants, antibiotics);
- stroke;
- multiple sclerosis.
Physiology of disease development (pathogenesis)
The pathogenesis of the disease is worth careful consideration. Roughly speaking, the transmission of nerve impulses can be compared to the movement of current through wires. All of them enter the brain, where they are transformed and “descend” back to the executive organs and systems: hormones and enzymes are released, various movements are carried out, etc.
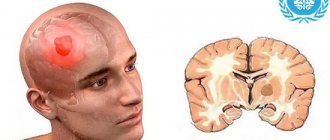
What is epilepsy and why does this disease begin? An epileptic seizure begins with strong overexcitation of nerve cells (neurons) in a certain area or in both hemispheres of the brain. Epilepsy takes quite a long time to develop.
- First, there is a slow change in the functional properties of neurons.
- Creation of a set of neurons that produce powerful nerve impulses that are tens of times greater than normal brain activity. This is the so-called epileptic focus or pacemaker.
- The formation of the so-called epileptic system, which includes the focus in the brain itself (sometimes nearby structures) and the nervous chain of impulse transmission to the executive organs.
An attack of epilepsy begins as the energy necessary to form such strong “discharges” accumulates. If the blood supply to the brain cannot replenish such energy costs in the period between attacks, then symptoms of hypoxia increase, which are fraught with the development of dementia, sclerosis and other disorders of brain activity.
Symptoms of epilepsy
As already mentioned, a generalized attack is characterized by tonic (persistent, prolonged) and clonic (rapid) convulsions and loss of consciousness. Before an attack, a short hallucinatory clouding of consciousness often occurs, immediately preceding the attack. At the onset of the tonic phase, the patient screams (as the muscles of the larynx contract), loses consciousness, bites his tongue and falls due to convulsions that begin throughout the body and limbs. There is a disturbance in pupillary reactions to light, cessation of breathing, pallor, and then cyanosis of the face.
A partial (minor) attack is a short-term clouding of consciousness. The patient remains on his feet, but his face turns pale, his eyes become glassy, and clonic spasms of individual muscles may be observed.
Symptoms of epilepsy: seizures and loss of consciousness.
It is impossible not to mention such a life-threatening condition as status epilepticus. We can say that this is a non-stop attack, woven from a series of seizures, without clearing consciousness. In this condition, it is necessary to immediately begin therapeutic measures.
Types of attacks
An epileptic seizure is a transient clinical manifestation of pathological excessive or synchronous neural activity of the brain (conceptual definition of an epileptic seizure, ILAE, 2005)
Seizures do not always mean that a person has epilepsy unless the diagnostic criteria for epilepsy are met. Because there are a number of conditions that may be associated with paroxysmal events that can mimic seizures/epilepsy, they should be carefully excluded.
A generalized attack is defined as one that occurs at a specific point and spreads rapidly through two-way networks. Such bilateral networks may include cortical and subcortical structures, but not necessarily the entire cortex. Although individual seizures may be localized, location and lateralization are not consistent from seizure to seizure.
Generalized seizures are divided into the following types:
With motor onset:
- tonic-clonic and their variants;
- tonic;
- atonic;
- myoclonic;
- myoclonic-atonic;
- epileptic spasms.
With non-motor onset:
- typical absence seizures;
- atypical absence seizures;
- myoclonic;
- absence seizures with myoclonus of the eyelids.
Generalized tonic-clonic seizures are bilateral and symmetrical generalized motor seizures that occur with loss of consciousness. A tonic-clonic seizure consists of a tonic (bilateral increased tone from a few seconds to several minutes) and then a clonic phase (bilateral sustained rhythmic jerking), usually in that order, but there are variations such as clonic-tonic-clonic and myoclonic-tonic. clonic.
Clonic seizures are seizures with bilateral, sustained rhythmic jerking and loss of consciousness. They differ from repeated serial myoclonic attacks by the rhythmicity of twitching with loss of consciousness. Recurrent serial myoclonic seizures (eg, myoclonic status epilepticus) are associated with irregular jerking, often with partially preserved consciousness.
In a generalized seizure with motor onset, asymmetries such as head and eye deviation may occur, but if consistent focal features are observed from seizure to seizure, consider focal bilateral tonic-clonic seizure or focal bilateral motor seizure.
An atonic attack is characterized by a sudden loss or decrease in muscle tone without visible preceding myoclonic or tonic signs. Atonic seizures are very brief (less than 2 seconds) and may involve the head, trunk, or extremities. Atonic seizures often occur in people with cognitive impairment.
Atonic seizures are one of the types of seizures that lead to falls like a drop attack. Other causes of such falls are myoclonic seizures (especially in young children), tonic and myoclonic-atonic seizures.
A myoclonic attack is manifested by a single or series of brief muscle contractions. Each contraction usually lasts milliseconds. Myoclonic status epilepticus is characterized by ongoing (more than 30 minutes) irregular jerking, often with partially preserved awareness. These two features distinguish status myoclonic epilepticus from generalized clonic status, in which consciousness is lost and the twitching is continuous and rhythmic.
Myoclonic-atonic seizure - a myoclonic seizure followed by atonic manifestations. Sometimes a series of myoclonic contractions occurs before atonia. The head and limbs are involved, usually resulting in a rapid fall. The myoclonic contraction may be brief.
An epileptic spasm appears as a sudden flexion, extension, or combined flexion-extension of the trunk muscles, lasting 1-2 seconds, that is, longer than a myoclonic seizure (lasts milliseconds), but not as long as a tonic seizure (lasts more than 2 seconds). Spasms are usually serial, often upon awakening. Subtle spasms can only be manifested by moving the chin, grimacing or nodding the head. Spasms can be bilaterally symmetrical, asymmetrical or unilateral, depending on the generalized or focal onset of the attack.
Epileptic spasms are usually serial (several in a cluster); if they are single, you need to think about other types of seizure.
Epileptic spasms may occur with a generalized, focal, or unknown onset of the attack. They may also occur not at the beginning of the attack, but later. Rapid diagnosis and relief of epileptic spasms promotes better developmental outcomes in young children. The focal onset of epileptic spasms is of particular importance, since identification of the structural cause allows planning curative surgical treatment. The focal origin of epileptic spasms is suggested by asymmetry of the motor features of the seizure (especially with initial spasms in a cluster), head/eye rotations, focal emphasis of the interictal or ictal EEG, and the presence of a focal structural abnormality of the brain.
Typical absence seizures are generalized seizures with a sudden onset and loss of consciousness that can vary in severity. Memory of events is usually impaired during an attack, although there may be some retention of attention, especially in adolescents. Clonic movements of the eyelids, head, eyebrows, chin, perioral or other parts of the face may occur, most often at a frequency of 3 Hz. Myoclonus of the limbs is rare. Oral and brachial automatisms are frequent. Perseveration of behavior may occur before an absence seizure. Status epilepticus absence seizures are also possible.
Isolated absence seizures lasting more than 45 seconds or absence seizures with a postictal phase are considered focal seizures.
The onset of absence seizures before the age of 4 raises concerns about a genetic mutation associated with glucose transporter deficiency (GLUT1).
Atypical absence seizures have a less abrupt onset and loss of consciousness than typical absence seizures. They often have other features: loss of muscle tone in the head, trunk or limbs (often a gradual decline) and mild myoclonic contractions. Atypical absence seizures often occur in people with cognitive impairment. Loss of consciousness may be minimal; if the patient continues to perform activities during absence seizure, he performs them more slowly or with errors.
These seizures may be difficult to recognize in a patient with ongoing slow (less than 2.5 Hz) generalized spike-wave EEG, and careful correlation between the EEG and clinical status is recommended.
Myoclonic absence seizures are rhythmic myoclonic shaking of the shoulders and arms with tonic abduction and progressive raising of the arms during an attack. Myoclonic jerks are usually bilateral, but can be unilateral or asymmetrical. Perioral myoclonus and rhythmic shaking of the head and legs may occur. The attacks last 10–60 seconds and usually occur daily. The level of awareness varies from complete loss to remaining conscious.
Absence seizures with myoclonus of the eyelids are short-term, repeated, often rhythmic, rapid (4-6 Hz) myoclonic twitching of the eyelids with simultaneous upward deviation of the eyeballs and throwing back of the head. The attacks are usually very short (less than 6 s), with several attacks occurring daily. Significant meaningfulness is retained.
If during an attack there is myoclonus and abduction of the upper limbs, myoclonic absence must be assumed.
Focal seizures are defined as originating from networks limited to one hemisphere. They can be highly localized or more widely distributed. Focal seizures may arise from subcortical structures. For each seizure type, ictal onset is consistent from one seizure to the next, with a preferred distribution pattern that may involve the ipsilateral and/or contralateral hemisphere. The semiology (symptoms/signs) of an attack allows for the identification of the specific brain region or lobe or hemisphere involved in the onset and spread of the attack.
A seizure is classified as focal if it is truly a focal epileptic seizure and conditions that mimic it are excluded.
The classification of focal attacks is carried out in two stages. Initially, the seizure is classified according to the level of awareness, as this is critical for safety and independence in daily life. If awareness becomes less pronounced at any time during an attack, the attack is a focal attack with decreased awareness.
Because the first seizure symptom/sign is the most useful feature for identifying the regional brain network in which the seizure originates, focal-onset seizures are also classified by their first seizure-onset symptom, even if it is not the most prominent feature of the seizure as a whole.
Therefore, the following signs have been approved for the classification of focal seizures:
- awareness or decreased awareness;
- motor onset;
- non-motor onset;
- sensory attack;
- focal cognitive seizure;
- focal emotional attack;
- focal vegetative attack;
- focal seizure with cessation of activity.
Focal seizures can spread widely throughout the brain, involving bilateral networks including cortical and subcortical structures, resulting in a tonic-clonic seizure with loss of consciousness. This type of seizure is known as a focal tonic-clonic seizure.
In addition to the initial symptom at the onset of the attack, additional symptoms/signs may occur during the course of the attack and reflect regional networks involved in the origin or propagation of the attack. Once a seizure has been classified by level of awareness and pattern of seizure onset, these additional relevant features are noted as descriptors .
Suggested steps for classifying focal seizures.
- Determine whether seizure onset is focal, considering all available relevant supporting information (seizure videos, EEG, MRI, and other test results) using the 80% confidence level. If this level of confidence is not achieved, the seizure should be considered as having an unknown onset or as unclassifiable if the available supporting information is incomplete.
- Decide whether there is awareness or reduced awareness (focal seizure with awareness or focal seizure with reduced awareness). Mindfulness requires a person to be fully aware of themselves and their surroundings during an attack, even if they are motionless. If awareness deteriorates at any time during an attack, the attack is considered to be focally impaired. If the degree of awareness is not specified, the seizure is a focal seizure with an unspecified degree of awareness.
- An attack is also classified according to the nature of its onset, which can be subjective or objective. This may be a motor or non-motor feature.
- then added as descriptors , which contribute to understanding the regional network in the brain involved in the initiation or propagation of seizures.
A motor-onset seizure involves motor activity (movement) and can be caused by either an increase or decrease in contraction of a muscle or muscle group. Depending on the muscle groups involved and how they are affected, the motor features of the motor onset of a seizure may be simple or more complex.
Types of seizures with motor onset
Focal clonic seizure - the movement is associated with a constant rhythmic jerking, and may involve a distal limb, one limb, or one side of the body. The twitching can spread and involve parts of the body according to their representation in the motor cortex (according to the homunculus), a phenomenon known as the Jacksonian March.
A focal hemiclonic seizure, where sustained rhythmic jerking rapidly involves one side of the body at the onset of the seizure, is an important marker for recognizing certain epileptic syndromes, such as Dravet syndrome and age-limited neonatal seizures.
A focal tonic attack is an increase in muscle tone, usually lasting from a few seconds to several minutes.
A focal motor attack with dystonia is a sustained contraction of agonist and antagonist muscles with the performance of athetoid or twisting movements, with the formation of a non-physiological position.
A focal myoclonic seizure is a single or short cluster of muscle contractions (jerks), each jerk usually lasting milliseconds.
A focal atonic seizure is a sudden loss or decrease in muscle tone without obvious preceding myoclonic or tonic activity, usually lasting more than 500 milliseconds but less than 2 seconds. It may involve the head, trunk, jaw, or limb musculature.
Focal motor attack with paresis/paralysis - the onset of the attack is characterized by weakness or complete paralysis of individual muscles or a group of muscles.
Focal epileptic spasm is a sudden flexion, extension or mixed flexion-extension of muscles, lasting 1-2 seconds, usually serial.
Focal hyperkinetic seizure - This type of seizure involves movements of the proximal limb or axial muscles, causing large-amplitude irregular movements such as pedaling, pelvic rocking, jumping, pumping and/or twisting movements.
A focal seizure with automatisms is a coordinated, repetitive motor activity that often resembles conscious movement but is carried out unconsciously. They are often found during attacks with loss/reduction of awareness, but can also occur in conscious states. Focal seizures with automatisms can be further described using the following descriptors:
- orofacial: lip smacking, wrinkling, chewing, swallowing, tongue flicking, blinking;
- manual: unilateral or bilateral, tapping, manipulating or searching movements of the hands;
- pedaling: bilateral or unilateral leg/foot movements, may include stepping, walking or running; the movement is more similar to normal movements in amplitude and less rapid compared to the movements observed with focal hyperkinetic seizures involving the legs;
- perseverative: the movement consists of an inappropriate continuation of the pre-attack movement;
- vocal: single or repeated sounds such as screams or grunts;
- verbal: single or repeated words, phrases or short sentences;
- sexual: sexual behavior;
- other: automatisms may include head nodding, undressing, and a number of other automatic movements.
Focal attack with dysarthria / antarthria - the onset of the attack is characterized by difficulty articulating speech due to impaired coordination of the muscles involved in speech production. The functions of active and passive speech are intact, but speech is poorly articulated and incomprehensible.
A focal seizure with negative myoclonus is a sudden interruption of normal tonic muscle activity lasting 500 milliseconds or less, without evidence of previous myoclonus. Seen in the epileptic syndrome of atypical childhood epilepsy with centrotemporal adhesions, where the upper limbs (or facial muscles) are affected by a localized, transient interruption of normal muscle tone. The interruption of muscle tone is briefer than in a focal atonic attack.
Focal motor attack with version - beginning with a prolonged, forced conjugate ocular, head and / or trunk rotation or lateral deviation from the central axis. It is important to determine sideness as it helps determine hemispheric lateralization, for example a seizure may be a focal motor seizure with a rightward version of the eyes and head.
Focal motor bilateral seizure - seizure begins in one hemisphere, but quickly involves bilateral muscle groups when seizures occur. Some subtypes of frontal seizures have bilateral motor signs at onset, often with an asymmetrical position. Typically, there is extension of the upper limb (at the elbow) contralateral to the hemisphere of seizure onset (often flexion of the fist and wrist) and flexion of the ipsilateral upper limb at the elbow. This type of grip is also described as the "fencer's position" or "figure 4". Awareness may be maintained during bilateral movement, leading to misdiagnosis of a non-epileptic seizure. These seizures may progress to a focal seizure, leading to a bilateral tonic-clonic seizure.
Epilepsy partialis continua
Epilepsia partialis continua refers to recurrent focal motor seizures (typically affecting the arm and face, although other parts of the body may be involved) that occur every few seconds or minutes over extended periods (days or years). Focal motor signs may appear as a Jacksonian march. Todd's paresis may occur in the affected part of the body.
Types of seizures with non-motor onset
A focal sensory attack involves the sensation experienced by the patient at the onset of the attack without objective clinical signs obvious to the observer. Focal sensory seizures can be further described using the following descriptors:
- Focal somatosensory attack - characterized by sensory phenomena including tingling, numbness, sensations similar to an electrical current, sensations such as pain, a feeling of movement or the desire to move. These seizures are associated with involvement of the sensorimotor cortex.
- Focal sensory visual seizure - characterized by elementary visual hallucinations such as flashing or flickering lights/colors or other shapes, simple drawings, scotomas, or amaurosis. More complex visual hallucinations, such as seeing formed images, are considered a focal cognitive seizure. Focal sensory visual seizures originate in the occipital lobe.
- Focal sensory auditory attack - characterized by elementary auditory phenomena, including buzzing, ringing, percussive or single sounds. More complex auditory hallucinations, such as voices, are considered focal cognitive seizures. Focal sensory auditory seizures occur in the auditory cortex in the lateral superior temporal lobe.
- Focal sensory olfactory attack - characterized by olfactory phenomena - usually a smell, often unpleasant. These seizures are associated with mesial temporal or orbitofrontal regions.
- Focal sensory taste attack - characterized by taste phenomena, including sour, bitter, salty, sweet or metallic tastes, occurring in the parietal regions (operculum and insula).
- Focal sensory vestibular attack - characterized by symptoms of dizziness, torsion, or a feeling of spinning. These seizures involve the parietal cortex, the temporo-parieto-occipital junction, or the parietotemporal cortex.
- hot and cold sensory attack - characterized by sensations of heat and then cold.
- Focal sensory attack with sensation in the head - characterized by a sensation in the head, such as mild dizziness or headache.
A focal cognitive attack involves a change in cognitive function (in the form of a deficit or a productive trait, such as violent thinking) that occurs at the onset of the attack. To be classified as a focal cognitive seizure, the change in cognitive function must be specific and disproportionate to other aspects of cognition because all cognitive functions are impaired in a focal cognitive seizure. Characterizing focal cognitive seizures may require specific testing early in the seizure. Focal cognitive seizures can be further described using the following descriptors:
- Focal cognitive attack with expressive dysphasia/aphasia —begins with an inability to speak, in a lucid patient who knows what he wants to say but cannot express it. This type of seizure should be distinguished from a focal motor seizure with dysarthria/anarthria, in which the patient speaks but the speech is poorly articulated (speech motor disorder).
- Focal cognitive attack with anomia is a specific difficulty in naming everyday objects.
- Focal cognitive attack with receptive dysphasia/aphasia – the attack begins with an inability to understand language in the absence of general confusion. It appears during attacks from the parietotemporal lobe of the dominant hemisphere.
- Focal cognitive attack with auditory agnosia - characterized by an inability to recognize or differentiate sounds/words or associate them with their meaning. For example, a person may hear a beep, but may not recognize that it is the sound of a telephone ringing.
- Focal cognitive seizure with conductive dysphasia/aphasia —begins with an inability to repeat audible speech due to an inability to encode phonological information, in establishing intact auditory perception (full understanding of what is heard), and mild speech production.
- Focal cognitive attack with dyslexia/alexia - the onset of attacks is associated with an inability to read due to impaired comprehension of written words, manifested in attacks from the parietotemporal lobe of the dominant hemisphere.
- Focal cognitive seizure with memory impairment —begins with an inability to retain events that occur during the seizure, while other cognitive functions and awareness are preserved during the seizure.
- Focal cognitive attack with déjà vu/jamais vu – characterized by memory disturbances such as feelings of familiarity (déjà vu) and unfamiliarity (jamais vu).
- Focal cognitive seizure with hallucination —characterized by complex sensations without the presence of external sensory stimuli, these may be visual, auditory, or involve other sensory modalities, without alteration of awareness. Sensory phenomena may be accompanied by an associated emotion or interpretation, for example the visual image formed may be accompanied by fear or may be experienced as stalking or paranoia (i.e. with unfounded suspicion/distrust).
- Focal cognitive attack with illusion - characterized by a change in actual perception, including visual, auditory, somatosensory, olfactory and/or gustatory phenomena, without a change in consciousness.
- Focal cognitive attack with dissociation - characterized by the experience of detachment from awareness of oneself or the environment.
- Focal cognitive attack with violent thinking - characterized by the presence of intrusive thoughts, ideas, or a stream of thoughts that occur at the onset of the attack. This is a rare type of seizure seen in seizures originating from the frontal lobe.
- Focal cognitive attack with dyscalculia/acalculia - characterized by difficulty completing or understanding a mathematical calculation, originating in the parietotemporal lobe of the dominant hemisphere.
- Focal cognitive attack with dysgraphia/agraphia - characterized by difficulty writing. This type of seizure originates from the parietotemporal lobe of the dominant hemisphere.
- Focal cognitive seizure with left-right confusion - characterized by an inability to distinguish between right and left at the onset of the seizure, originates in the parietotemporal lobe of the dominant hemisphere.
- Focal cognitive seizure with negligence - characterized by a unilateral inability to report or respond/orient to stimuli presented contralaterally. They originate from the contralateral hemisphere during attacks from the parietal lobe of the non-dominant hemisphere.
Focal autonomic seizures are characterized by changes in systems controlled by the autonomic nervous system, with or without being obvious to the observer. Focal autonomic seizures can be further described using the following descriptors:
- Focal autonomic attack with flutter/tachycardia/bradycardia/asystole.
- Focal autonomic attack with epigastric sensations (epigastric discomfort, emptiness, bloating, hunger - the sensation may rise to the chest or throat) or nausea/vomiting (or other gastrointestinal symptoms) - attacks with these features usually originate in the mesial temporal lobe.
- Focal autonomic attack with pallor/blushing.
- Focal autonomic attack with hypoventilation/hyperventilation/altered breathing.
- Focal vegetative attack with piloerection.
- Focal autonomic attack with erection.
- Focal autonomic attack with urge to urinate/defecate.
- Focal autonomic attack with lacrimation.
- Focal autonomic seizure with pupil dilation/constriction.
Focal emotional attacks are characterized by changes in mood or emotions, or the appearance of altered emotions, when an attack occurs. These emotional attacks may occur with or without objective clinical signs of an attack obvious to the observer. Focal emotional attacks can be further described using the following descriptors:
- Focal emotional attack with fear/anxiety/panic - characterized by the presence of fear, worry, worry or panic as an expressed or observable emotion at the onset of the attack. Due to the unpleasant nature of these attacks, patients may also have pre-anxiety about the attack. These seizures originate in the mesial temporal networks, especially the amygdala. They can be distinguished from panic attacks by the presence of changes in awareness, automatisms and other signs of epileptic seizures that occur in a stereotypical manner. They also differ from a focal autonomic attack with epigastric sensation, where the feature of the onset of the attack is an autonomic epigastric sensation and fear may be present as a secondary feature.
- Focal emotional attack with laughter (gelastic) - bursts of laughter or giggles, usually without the corresponding associated emotions of happiness and described as "joyless." This type of seizure is common in seizures originating in the hypothalamus (hypothalamic hamartoma), but can occur in seizures originating in the frontal or temporal lobes.
- Focal emotional attack with crying (dacrystic) - characterized by stereotypical crying, may be accompanied by lacrimation, a sad facial expression and sobbing. The subjective emotion of sadness may or may not exist. These attacks often accompany focal emotional attacks with laughter with a focus in the hypothalamic hamartoma. They can also occur with seizures originating in the frontal or temporal lobes. Crying is a rare feature of an epileptic seizure and is most often a symptom of a non-epileptic seizure.
- Focal emotional attack with pleasure - characterized by the presence of a positive emotional feeling of pleasure, bliss, joy, ecstasy. This is a rare type of seizure seen in seizures originating in the anterior insular cortex.
- Focal emotional attack with anger - characterized by the presence of anger, which may be accompanied by aggressive behavior. This is a rare type of attack; anger and aggression, if present, are mainly observed in the post-attack period. This type of seizure is localized in the prefrontal or mesial region of the brain. Focal emotional attacks with anger differ from hysterical and violent reactions in the absence of organized, purposeful aggressive behavior, their stereotypical development during each attack and the presence of other signs of an epileptic attack as the event unfolds.
A focal arrest seizure is characterized by a decrease in amplitude and/or speed or cessation of ongoing motor activity during the seizure. Because brief cessation of activity is common and difficult to identify at the onset of many attacks, the cessation should be persistent and dominant throughout the attack.
Focal seizure with evolution into bilateral tonic-clonic seizure.
A focal seizure may spread to involve wider brain networks, resulting in a bilateral tonic-clonic seizure. This was previously known as a "secondary generalized attack." Consciousness is impaired. Motor components in this situation include tonic and clonic signs. This type of seizure may occur after other types of focal seizures, such as focal motor, focal cognitive, focal sensory, or focal awareness seizures. Propagation through brain networks may be so rapid that the preceding focal seizure type is not detected. A focal seizure progressing to a bilateral tonic-clonic seizure can be distinguished from a generalized tonic-clonic seizure based on other evidence that is suggestive of a focal epilepsy/etiology, or an asymmetry may be seen in a focal seizure progressing to a bilateral tonic-clonic seizure (eg, version head/eyes on one side, asymmetrical amplitude of motor features), and this asymmetry is persistently observed from attack to attack.
Diagnosis of epilepsy
First of all, it is necessary to recognize the type of epilepsy (congenital or acquired). In the second case, to establish the primary disease. Interviewing the patient himself is a futile exercise, because... an epileptic seizure involves amnesia. Therefore, the importance of information provided by the patient’s family and friends increases.
What tests are required to diagnose epilepsy? First of all, electroencephalography (EEG), which reflects deviations in the electrical activity of the brain and records the epileptic focus. During the interictal interval, EEG indicators often do not differ from normal ones, so magnetic resonance imaging and computed tomography of the brain are additionally performed.
Diagnosis of epilepsy begins with electroencephalography
Diagnostic stages
At the first stage, a neuropathologist must conduct a clinical examination, which will determine the nature and localization of the disease and choose tactics for additional examination and treatment. An effective research method is radiography, which is used to determine the condition of the osteoarticular tissues of the spine. Magnetic resonance imaging allows you to see in more detail not only the bone, but also the spinal roots, blood vessels, cartilage tissue, ligaments and muscles. Among other additional methods used to study the neurology of the disease, homeopathy, reflexology, homotoxicology, manual therapy, acupressure, and Doppler ultrasound are popular.
The Neurology Research Center is developing methods for treating neurological diseases. Today, an integrated approach to treatment is widely used. It is aimed at eliminating the causes and alleviating symptoms. Neurological pathologies are mainly treated through the use of drug therapy. Additionally, rehabilitation and recovery techniques are used, including heat therapy, therapeutic exercises, kinesitherapy, acupuncture, therapeutic massage, physiotherapy and herbal medicine. In addition, there are special rehabilitation programs for patients.
You can protect your body from neurological disorders and prevent complications only by taking care of your health, which includes a healthy lifestyle, avoiding stress and undergoing periodic examinations with a neurologist.
Top 10 Broke Stars It turns out that sometimes even the biggest fame ends in failure, as is the case with these celebrities.
20 photos of cats taken at the right moment Cats are amazing creatures, and perhaps everyone knows this. They are also incredibly photogenic and always know how to be in the right place at the right time.
Contrary to all stereotypes: a girl with a rare genetic disorder conquers the fashion world. This girl's name is Melanie Gaydos, and she burst into the fashion world quickly, shocking, inspiring and destroying stupid stereotypes.
11 Weird Signs That You're Good in Bed Do you also want to believe that you please your romantic partner in bed? At least you don't want to blush and apologize.
9 Famous Women Who Have Fallen in Love with Women Showing interest in people other than the opposite sex is not unusual. You are unlikely to be able to surprise or shock anyone if you admit it.
Why do you need a tiny pocket on jeans? Everyone knows that there is a tiny pocket on jeans, but few have thought about why it might be needed. Interestingly, it was originally a place for storage.
Treatment of epilepsy
Treatment of epilepsy is based on the principles of timeliness, complexity, duration and continuity. It involves the constant use of anticonvulsants, which either completely eliminate seizures or make them much less frequent. Phenobarbital, Diphenin, Chloracone, Hexamidine (Primidon), Benzobarbital (Benzonal), Carbamazepine (Finlepsin, Zeptol) are used to relieve generalized seizures.
For partial seizures, Suxilep, Diazepam (Relanium, Sibazon), Encorate (Depakine, Valparin), the same Carbamazepine, Diphenin are used.
The effect of drugs on a particular patient is strictly individual. The duration of treatment, as a rule, is at least 2-3 years after the last generalized attack and 1.5-2 years after a partial attack. Normalization of the EEG is also an important criterion for discontinuing drug treatment. Drug therapy is not interrupted abruptly, it is done gradually by gradually reducing dosages.
The diet for epilepsy should include a minimum of salt, seasonings, cocoa, and coffee. Liquid consumption is limited, alcohol is excluded.
Emergency assistance to the patient directly during an attack should be aimed at preventing asphyxia. In Russian, it is necessary to ensure that the patient does not suffocate due to the retraction of the tongue or does not choke on vomit. It is also necessary to stimulate cardiac activity and stop seizures. To do this, you should empty the oral cavity of vomit, insert an air duct, and inject Cordiamin.
Signs preceding the onset of an attack
With epilepsy, the symptoms of which are complex partial seizures, sick people often feel their approach. If epileptic seizures occur rarely, then a few days before the seizure a person begins to experience periodic headaches, drowsiness, and attention disorders. However, the so-called aura most often manifests itself. It comes in several types:
- The sensory aura is accompanied by complex or simple visual hallucinations, in which a person can see flashes of lightning, bright shiny balls or ribbons, and the surrounding world is painted in bright colors. Sometimes there is limited lateral vision or temporary blindness. The sensory aura is also characterized by auditory hallucinations and the sensation of a foreign taste or smell.
- The mental aura is characterized by the appearance of a feeling of bliss, euphoria, or, conversely, causeless strong fear.
- Vegetative aura manifests itself in the form of changes in skin color (redness or pallor), tachycardia, a strong urge to defecate or urinate, the appearance of cold sweats, chills or fever. You may also experience pain in the abdomen, nausea, and increased salivation.
- Speech aura looks like distortion of speech, muttering.
- Motor aura is characterized by the appearance of automatic movements. This could be turning the head, chaotic movements of the hands, shifting objects, flicking switches. Then chewing, swallowing or sucking movements are added.
Typically, the warning signs of a complex partial seizure last a few seconds, but during this time the patient or his loved ones can take measures to ensure their safety. It is very important to know what can cause complications in a person with epilepsy. The onset of an attack can be caused by sharp unexpected sounds, bright flashing lights, rapid changes in images (for example, when watching a movie or other video), severe stress, smoking, drinking coffee, alcohol, drugs, and lack of sleep.
Symptoms and diagnosis
Acquired and congenital pathology usually manifests itself after fast running, consumption of alcohol, psychotropic and narcotic substances, in bright light, and stressful situations.
It occurs that epilepsy does not manifest itself for a long time, and in some cases, up to several years.
The attack usually occurs unexpectedly.
A patient with epilepsy after experiencing an attack, accompanied by convulsions, rapid breathing, involuntary urination, salivation, foam at the mouth, and fever, usually does not remember anything.
Before an attack, there are headaches, fatigue appears, there may be causeless constant changes in mood, unpleasant odors are felt, an untidy taste appears in the mouth, but this can occur without any kind of precursors.
Both congenital and acquired epilepsy can provoke hallucinations, the appearance of flashes of light in the eyes. During a seizure, the heartbeat quickens, the limbs of the body become numb, sharp pain may appear in them, and the patient feels cold. Then the convulsions begin.
During seizures, the patient falls, convulsions may begin to appear first in the limbs, and then disperse throughout the body. The pupils do not react to light. There is blueness or paleness of the skin, loss of consciousness, after which muscle relaxation and, possibly, sleep may occur.
In rare cases, respiratory arrest may occur.
During seizures, others need to protect the patient from sharp, hard objects and, if possible, hold him in order to prevent him from inflicting injuries of various kinds on himself.
It is best to insert a hard object into the oral cavity to avoid biting off the tongue, as well as it sticking into the nasopharynx, which can cause respiratory arrest. For the same purpose, the patient is recommended to lay his head to one side.
The duration of the attack ranges from 1 to 5 minutes.
So-called mild seizures, expressed in subtle twitching of the face and eyelids, are rare.
Particularly dangerous is status epilepticus, which is characterized by the presence of several seizures in a row and can lead to death.
In epileptics whose disease has become chronic, personality changes occur over time, expressed in the following emotional manifestations:
- begin to find fault with little things;
- selfishness begins to dominate over all human qualities;
- the sphere of interests is noticeably reduced;
- there is a constant change of mood;
- manifestations of the development of dementia occur;
- there are injuries on the tongue from his regular biting and other traces from self-inflicted injuries;
- strongly expressed fear, aggressiveness, and melancholy appear.
Two doctors can make an accurate diagnosis: a neurologist and a psychiatrist, based on laboratory examinations, medical history, descriptions of seizures; for a more accurate clinical picture, electroencephalography, tomography, X-rays and MRI can be prescribed.
Epileptic seizures
Among the periodic seizures in epilepsy are:
Generalized - begin with a loss of consciousness, develop as a result of excessive activation of the deep parts of the nervous tissue, with further involvement of the electrical activity of the structures of the entire brain. Generalized epileptic paroxysm occurs in several phases: initial, clonic (characterized by clonic convulsions), tonic, and the phase of loss of consciousness (after a generalized epileptic attack, loss of consciousness occurs, like stunning, or deeper; for some time after such a paroxysm, the patient is not awakened, then consciousness gradually returns).
Local seizures develop as a result of increased electrical activity in one area of the brain. The manifestations of such paroxysm will depend on the localization of the pathological focus and can be motor, sensory, autonomic or mental. A simple partial seizure is characterized by complete preservation of consciousness and lack of control over any of the body’s functions; accompanied by unusual sensations. A complex attack occurs against the background of impaired consciousness, for example, with a partial loss of it, which can be in the nature of stupor or stupor, combined with a lack of control over a particular part of the body. Possible nature of the violations: uncontrolled movements or imitation of purposeful movements (walking). Partial seizures, both simple and complex, can end in generalization. In this case, loss of consciousness will occur.
Causes of the disease, prevention and treatment
Acquired epilepsy differs from congenital epilepsy in that the latter is caused by a genetic predisposition.
The acquired causes are characterized by an adverse effect on the brain, forming an epileptic focus in one of its hemispheres, conducting an electrical impulse.
Precursors of the disease are various damage or inflammation of the brain.
Causes of acquired epilepsy:
- mechanical head injuries resulting in brain damage;
- infectious diseases, diseases of the cardiovascular system, as a rule, mainly after a heart attack;
- hypoxia in the fetus in the womb.
- tumor, cyst and hematoma of the brain;
- impaired metabolism;
- hypoxia and impaired blood supply to the brain;
- Down syndrome;
- side effect of strong medications.
Treatment of the disease
Epilepsy is an incurable disease. Unless it can go away on its own forever in adolescence. Drug treatment of epilepsy is aimed at minimizing the number of convulsive epileptic seizures. This is achieved by prescribing special drugs from the group of antiepileptic drugs.
Their action is based on inhibiting the activity of neurons in the focus of increased excitability in the brain, as well as blocking the spread of pathological impulses. A number of strict requirements are imposed on such medications. To achieve the desired effect, the medicine must be taken for a long time (at least 2 - 3 years). Therefore, the risk of developing side effects such as disruption of internal organs, drowsiness or confusion should be minimized.
In addition, when used regularly, the main active ingredient of the drug should not accumulate in the body and cause addiction or dependence. These requirements are met by the following:
- Carbamazepine and its analogues with the same composition are the “first choice” drugs for the treatment of almost all forms of epilepsy. The undoubted advantage of this medicine is the combination of anticonvulsant activity with a psychotropic effect. Therefore, after taking the pills, mood improves, social adaptation and performance improve. However, at the beginning of the course of treatment with Carbamazepine, complaints of dizziness, headaches, drowsiness, and disorders of the digestive system are noted. The dosage of the drug is selected individually. It depends on age, frequency and severity of epileptic seizures.
- Depakine, the active ingredient of which is sodium valproate. It enhances the effect of other anticonvulsants, which must be taken into account when prescribing a combination of several medications.
- A relatively new drug for the treatment of epilepsy is Lamotrigine or Lamictal. This remedy acts for quite a long time (about a day), in addition, when used, the sedative effect is less pronounced
Treatment of epilepsy in adults and children is the same, only the dosages of prescribed medications differ.
Previously, doctors used combinations of several antiepileptic drugs to treat epilepsy. However, recent studies have shown monotherapy to be more effective. Therefore, most neurologists take this tactic for treating epilepsy as a basis. The effectiveness of treatment is monitored by a doctor using a repeated EEG.
To improve cerebral circulation during hypoxia during the interictal period, drugs such as Actovegin, Piracetam, Pantogam, Gliatilin or Curantil are prescribed. The use of mild sedatives, for example Glycine, Seduxen, and valerian extract, is also indicated. Motherwort for epilepsy is considered a very effective remedy from the arsenal of herbal medicine, as it perfectly strengthens the nervous system, a decoction of shiksha, which has an anticonvulsant effect.
Treatment for status epilepticus is more complex and can only be done in hospital due to the risk of serious side effects. Drip administration of barbiturates, anesthetics, and magnesium injections are indicated. If the cause of epilepsy is a tumor in the brain, then the root cause of the disease is treated first.
However, it should be noted that a quarter of patients have a drug-resistant form of epilepsy that cannot be corrected with drugs. In such cases, the only option is surgery.
Symptoms and causes
Acquired or symptomatic epilepsy is a disease that occurs as a result of a situation that traumatizes brain cells. The causes of this form of the disease are:
- Head injuries. Concussions, bruises, and skull injuries can trigger the appearance of this disease.
- Childbirth. Complicated childbirth can lead to injury to the baby's head, the consequences of which can be acquired epilepsy in the child.
- Violation of intrauterine development. Epilepsy, which is not genetically characteristic of the child, can be caused by hypoxia (oxygen starvation) experienced in the womb.
- Addiction. Addiction to alcohol and drugs causes damage to neurons.
- Infectious diseases. Diseases affecting the central nervous system, such as meningitis, encephalitis.
- Stroke.
- Multiple sclerosis.
- Side effects of medications.
- Brain tumors.
The most common belief is that all people with epilepsy experience severe seizures. In fact, some patients may not experience seizures at all, or the seizures may be barely noticeable.
- Seizures with complete loss of consciousness. During such an attack, a person experiences convulsions of the whole body or individual parts of it, and involuntary urination is possible.
- Seizures with partial loss of consciousness. The attack is accompanied by convulsions, the person passes out for a while, then comes to his senses again, the shift is repeated several times.
- Seizures without loss of consciousness. A seizure can be accompanied by both strong and faintly noticeable convulsions, the person is completely conscious.
- Development of mental illness. With epilepsy, depression, hallucinations, and schizotypal disorders may occur.
- Dizziness, headaches, impaired spatial perception.
Also, it is worth noting that epilepsy can manifest itself in a latent form, without obvious external manifestations. In this case, it is possible to find out about the disease during a brain examination when lesions are detected.
After a traumatic situation, the disease can manifest itself both immediately and after a long period of time.
Epilepsy and psychosomatics
Convulsive syndrome cannot always be explained by physiological reasons. The onset of an epileptic attack in the absence of obvious provoking factors is often associated with psychosomatics. Especially if the onset of the disease occurs after 25 years of age. It is believed that certain behavioral patterns and mental reactions can, over time, lead to the development of epilepsy or episyndrome. The psychosomatics of the disease can be caused by various manias, phobias and fears. Constant mental stress can cause changes in nerve impulses, and over time, disruption of the electrical activity of the cerebral cortex. The psychosomatics of epilepsy may be associated with childhood trauma and domestic violence. A person who leads a reclusive lifestyle gradually loses social adaptation and contacts with people often subsequently develops epilepsy caused by psychosomatics. In such a person, individual brain functions simply atrophy over time.
Types of acquired epilepsy
Symptomatic epilepsy is divided depending on the location of the brain lesion. Possible forms:
- Temporal lobe epilepsy is the most common. It is interesting that in case of temporal lobe epilepsy, the epileptogenic focus can be located in other lobes of the brain, while the discharge spreads to the temporal lobe from a focus located in another area.
- Frontal lobe epilepsy is a difficult form of the disease, characterized by frequent attacks and the possibility of unfavorable trends in the development of the disease.
- Parietal lobe epilepsy is the rarest form of symptomatic epilepsy. With this type of disease, the following are possible: pain of varying strength during attacks, disturbances in temperature perception, sudden throbbing pain in the extremities.
- Epilepsy of the occipital lobe - characterized by: migraines, hallucinations, parasthesia (numbness, tingling) in the eye area, as well as the spread of epileptic activity to other areas of the brain.
- Syndromes with attacks that are provoked by specific factors.
- Kozhevnikov syndrome - occurs in children and adolescents and often appears with encephalitis.
Congenital and acquired epilepsy: causes, signs and differences
According to statistics, every hundredth inhabitant of the Earth suffers from epilepsy. The disease is characterized by increased activity of neurons in the brain, as a result of which a person develops repeated seizures.
Is epilepsy a congenital or acquired disease? 70% of cases of pathology are congenital; the occurrence of the disease is based on a hereditary predisposition.
The acquired form is a consequence of brain damage (trauma, infection, tumor). Both types of illness have similarities and differences.
Basic Concepts
An epilepsy attack occurs due to increased electrical activity of nerve cells.
Epilepsy is a chronic disease of the nervous system, characterized by repeated epileptic seizures in the form of motor, sensory, autonomic and mental manifestations.
An epileptic seizure (attack) is a transient condition that occurs as a result of the development of electrical activity of nerve cells (neurons) in the brain and is manifested by clinical and paraclinical symptoms, depending on the location of the source of the discharge.
The basis of any epileptic seizure is the development of abnormal electrical activity of nerve cells that form a discharge.
If the discharge does not go beyond its focus or, spreading to neighboring areas of the brain, encounters resistance and is extinguished, then in these cases partial seizures (local) develop.
In the case when electrical activity affects all parts of the central nervous system, a generalized attack develops.
In 1989, an international classification of epilepsies and epileptic syndromes was adopted, according to which epilepsies are divided according to the type of attack and etiological factor.
- Local (focal, localization, partial) epilepsies:
- Idiopathic (rolandic epilepsy, reading epilepsy, etc.).
- Symptomatic (Kozhevnikov’s epilepsy, etc.) and cryptogenic.
This type of epilepsy is diagnosed only if, during examination and obtaining electroencephalogram (EEG) data, the local nature of paroxysms (attacks) is revealed.
- Generalized epilepsy:
- Idiopathic (benign familial seizures of newborns, childhood absence epilepsy, etc.).
- Symptomatic (West syndrome, Lennox-Gastaut syndrome, epilepsy with myoclonic-astatic seizures, with myoclonic absences) and cryptogenic.
Seizures in this form of epilepsy are generalized from the very beginning, which is also confirmed by clinical examination and EEG data.
- Indeterminate epilepsy (neonatal seizures, Landau-Kleffner syndrome, etc.).
Clinical manifestations and changes in the EEG have features of both local and generalized epilepsies.
- Special syndromes (febrile convulsions, seizures that occur during acute metabolic or toxic disorders).
Epilepsy is considered idiopathic if an external cause has not been identified during examination, so it is also considered hereditary.
Symptomatic epilepsy is diagnosed when structural changes in the brain and diseases are found, the role of which in the development of epilepsy has been proven.
Cryptogenic epilepsies are epilepsies for which the cause could not be identified, and there is no hereditary factor.
Prevention
As such, no specific prevention has been developed. But there are some recommendations to minimize risks. Among them:
- Avoiding stress. If possible. If your work or character and lifestyle involve constant high emotional and mental stress, it is recommended to master relaxation techniques, and if necessary, you should consult a psychotherapist.
- Adequate physical activity. No overload. Physical inactivity is also not desirable, although it does not play such a catastrophic role.
- Full sleep. At least 7 hours per night for an adult, at least 8 (mandatory) for a school-age child. 8-9 for very young patients.
- Complete nutrition. It is better to discuss the diet with a nutritionist. It should contain a sufficient amount of B vitamins to maintain the nervous system in good shape.
- Timely treatment of all somatic diseases, if any. Without exception. Cardiovascular pathologies, diseases of the endocrine system, and the musculoskeletal system at the level of the cervical spine are especially dangerous.
- Avoiding sudden changes in temperature.
- Regular preventive examinations.
Risk factors for developing epilepsy
- Hereditary history (the role of genetic factors in the development of epilepsy has been reliably established);
- Organic brain damage (intrauterine infection of the fetus, intrapartum asphyxia, postnatal infections, brain injury, exposure to toxic substances);
- Functional brain disorders (impaired sleep/wake ratio);
- Electroencephalogram (EEG) changes;
- Febrile seizures in childhood.
The clinical picture of any epilepsy consists of seizures, which are diverse in their manifestations. There are two main types of seizures: generalized and partial (motor or focal).
In order not to repeatedly describe the clinical picture of the same seizures in different types of epilepsy, we will consider them at the beginning.
What disease is this
Is epilepsy a congenital or acquired disease? Epilepsy can be congenital (idiopathic) or acquired (symptomatic). Heredity is to blame for the first one.
The patient has a genetic disorder in the brain structures responsible for the processes of inhibition and excitation. The development of the disease can be provoked by fetal hypoxia, intrauterine infections, and birth injuries.
The culprits of acquired pathology are various effects on the brain in the form of injuries or diseases. The consequence of this is the formation of an epileptic focus.
Up to a certain point, the body fights and extinguishes unnecessary impulses.
Diagnosis of the disease
Diagnosis of epilepsy is carried out very carefully and begins with a medical history.
It is necessary to understand the cause of symptomatic epilepsy.
It is also important for the doctor to know the details of how seizures occur, whether there are perception disturbances or other negative consequences that can be caused by epilepsy.
The following examinations are prescribed:
- MRI is necessary to detect or exclude the presence of tumors, other diseases of the nervous system, and abnormalities of brain development.
- Electroencephalography records the electrical activity of the brain and is an examination that is carried out continuously throughout the disease. EEG helps: observe changes that occur during the course of treatment, identify deterioration of the condition, determine the activity of lesions.
- Video-EEG monitoring. This study allows you to observe epileptic activity during an attack and record changes in activity throughout the day. During such an examination, the patient remains in the ward for several days under camera surveillance. EEG recording occurs continuously automatically.
- Positron emission tomography. The examination allows you to assess the state of the brain and predict the possible course of the disease.
Epilepsy is a fairly common disease.
Symptomatic epilepsy is one of the forms of the disease. What it is expressed in and how to treat it, read on our website. Is it possible to completely cure epilepsy in childhood? This question is often asked by young mothers. You will find the answer in this article.
Clinical course of epilepsy
A characteristic feature of the clinical picture of the disease is that each form of this disease is characterized by a typical course of epileptic seizures. In the period of time between seizures, signs of epilepsy in adult men, women and children are practically absent, people can lead a normal lifestyle and feel quite normal.
In some cases, during the interictal period, the disease that caused the development of epilepsy manifests itself (tumor, stroke, consequences of traumatic brain injury). Symptoms of oxygen starvation of the brain may also increase, which manifest themselves in increased fatigue, frequent headaches, irritability, suspiciousness, and depression. This condition in old age can lead to personality changes and dementia.
The main symptoms of epilepsy are seizures. Their frequency is different for each patient. Some people may experience attacks 1-2 times a week, while others may experience them much more often.
The main general signs of epileptic seizures are:
- The suddenness of their beginning and ending.
- Short duration (from a few seconds to 5 – 6 minutes). If they are not accompanied by pronounced symptoms (convulsions or screams), then they may not be noticed from the outside. By the way, this is one of the reasons for delays in seeing a doctor and starting treatment.
- Regularity of repetition.
- Typical clinical picture for each specific form of epilepsy.
If seizures are too frequent (several times a day), there is a high likelihood of developing status epilepticus. Its main symptom is the repeated repetition of attacks, and between them people do not regain consciousness. This condition threatens death and requires immediate hospitalization and qualified medical care.
Status epilepticus must be distinguished from serial epileptic seizures, when in the period of time between them a person is fully aware of where he is and what is happening to him. However, this is fraught with serious damage to the brain, since with frequently recurring attacks, the state of the nervous system and other organs does not have time to return to normal.
Prevention and treatment
Treatment includes many measures, which include:
- taking medications;
- intramuscular and intravenous administration of drugs to stabilize brain function;
- avoiding contact with seizure triggers (alcohol, drugs, certain medications, bright flashing lights);
- exclusion of head injuries;
- surgical intervention;
- treatment of concomitant disease.
Also, when treating epilepsy, it is necessary to follow a daily routine and diet, engage in acceptable physical activity, and try to avoid stress and overexertion of the body. It is important to regularly see your treating epileptologist and undergo brain examinations. A visit to a psychotherapist may be necessary if the illness is accompanied by mood disorders or hallucinations to prescribe additional medications.
Trying to cure a disease at home or using traditional medicine is dangerous to your health! But taking vitamins and additional nutrients (omega-3) helps improve the condition.
- timely treatment of infectious diseases and head injuries;
- vaccinations (encephalitis);
- observation by an oncologist;
- prevention of intoxication.
The symptomatic form of epilepsy is not hereditary.
At the same time, it is important to monitor the intrauterine development of the fetus and the health of the mother in order to try to exclude the possibility of the disease developing in the child during pregnancy.
Epilepsy is one of the most common neurological diseases. But this disease can be controlled; modern medicine allows you to get rid of its negative manifestations. Many people with epilepsy lead active lives, drive cars and do things they love.
Is it possible to predict epilepsy in a child? Is epilepsy inherited? You will find answers to these questions in this article.
Read about what focal epilepsy is and how it manifests itself in this material.
Disease prognosis
There is still a misconception that epilepsy inevitably leads to a decrease in intelligence. In fact, cognitive decline occurs only in rare cases. After the first attack, with a maximum degree of probability, a favorable prognosis can be made. Today, epilepsy is no longer as dangerous as it used to be; it is not considered an incurable disease. The achievements of modern medicine make it possible to ensure normal life and health for more than 70% of patients with this diagnosis
However, it is important to realize that epilepsy is not a joke disease; in some cases it can be fatal. A person may die due to an unsuccessful fall during a generalized attack or due to asphyxia due to saliva or blood entering the lungs
The most dangerous for human life is status epilepticus - several consecutive attacks. Increased muscle activity greatly increases the load on the heart, and impaired breathing leads to hypoxia and increased acidity. All these processes can cause swelling of the brain, disrupt blood microcirculation, and lead to tissue necrosis. This state of the body and irreversible neurochemical processes during epistatus lead to the death of a person.
First aid for a patient with an epileptic seizure
Parents and loved ones of a person suffering from epilepsy need to know the rules for helping in the event of an epileptic attack at home (it’s better to even look at the corresponding photos and videos on the Internet, read forums).
- First of all, you need to get rid of tight clothing, especially in the throat area, remove jewelry and watches.
- Move the person or remove glass and stools away to protect the epileptic from shock and injury.
- Tilt your head to the side to prevent saliva from entering the airways and swallowing your tongue.
- If convulsions are accompanied by vomiting, the patient must be turned to one side and held in this position.
- Stay close until the attack ends, and then, if necessary, change clothes, warm you up and let you sleep.
What should you not do if you have epilepsy? Under no circumstances should you try to open your jaws with a wooden spatula or any other object during an attack, or give medications in liquid form. If necessary, medications can only be administered by injection.