What is postpartum depression?
Postnatal or postpartum depression, what is it for the common man? Just the whims of a young woman and the desire to attract attention. In reality, this is an unbalanced state of the body and psyche, which turns the life of new parents into hell. However, it often happens that the child’s father does not notice anything, and the woman tries to cope on her own, sliding into the abyss of despair and hopelessness or losing her mind on an emotional swing.
The whirlpool of emotions captures and covers your head. One minute the mother was ready to cry out of tenderness for the baby, but a minute later she experiences the deepest melancholy and the recent “sweet tears” are already burning with their impossible bitterness. Postpartum depression is not just a reaction to a recent event, but a loss of support and stability.
This type of depression is not only unbalanced and uncomfortable, it harms the newborn baby. Clinical depression requires mandatory medical intervention. Therefore, it is important to recognize the disease among other disorders that you can cope with yourself or with the help of loved ones. There are several such disorders:
✔️ Blues, melancholy (postpartum). Occurs in 70% of women who have recently given birth. Appears in the first week after birth. The mother experiences tearfulness, self-doubt, and fear for the baby. The reason for this condition lies in a sharp change in hormonal levels. It is aggravated by stress due to new conditions. The duration of the blues is 1-2 weeks. It does not require the intervention of specialists.
✔️ Depression (postpartum). A tendency to this phenomenon was noted in 13% of women who went through childbirth. The first symptoms are noted within several weeks after this event. If a woman is in this state for more than two weeks, then there is a high probability of depression. The symptoms resemble melancholy, but are more vivid in nature and affect not only the psyche, but also physiology.
✔️ Psychosis (postpartum). This condition is observed extremely rarely, 1 in 1000. The onset of the disease is noticed in the first weeks after the event. This is a serious mental state, aggravated by depression, which is accompanied by hallucinations, confusion, and a tendency to harm oneself, a child, or loved ones. In this case, the woman needs to be monitored by a psychiatrist.
Disease prevention
Prevention is necessary not only in the maternity hospital and after the birth of the child, but also at the stage of planning a pregnancy by a couple and throughout the entire period of dispensary observation by a gynecologist at the antenatal clinic, so that the young mother herself can cope with postpartum depression.
Depending on the tasks at each stage, primary and secondary prevention are distinguished. The objectives of primary prevention are a careful study by an obstetrician-gynecologist of the anamnesis (history) of a woman’s life, her heredity, and social status. He should conduct psychoprophylactic preparation for childbirth, familiarize the woman and her husband with the sensations that she will experience during pregnancy and childbirth, with the possible development of the “postpartum blues” syndrome and the “grief reaction under severe stress”, explain their non-pathological nature and familiarize with control measures.
In addition, a pregnant woman needs to be taught psychological auto-training, explain the importance of communicating with her friends, other pregnant and young mothers, the importance of maintaining a balanced diet and daily routine, walking in the fresh air, and also give recommendations on physical activity and gymnastic exercises.
The objectives of secondary prevention are to teach the pregnant woman how to deal with postpartum depression at home. If there is a history of depression, special attention is paid to changes in her self-esteem, conducting psychoeducational conversations with relatives and people close to the woman in order to create for her a supportive family atmosphere, emotional and physical support, favorable living conditions and comfort. Secondary prevention is carried out by a general practitioner or family doctor.
If alarming symptoms of the disease persist for 2–3 weeks, as well as with a mild degree of pathology, the woman should be provided with medical assistance from a family doctor or psychiatrist together with an obstetrician-gynecologist in the form of non-drug therapy.
How does postpartum depression manifest?
Of course, this condition has its own signs and symptoms. It is not necessarily expressed in a bad or depressed mood, but most often this is what happens. How does postpartum depression manifest itself?
- Depressed mood (as already mentioned);
- Feelings of guilt and fear for the baby;
- Overprotection or vice versa, distancing from the newborn;
- Loss of concentration, absent-mindedness;
- Apathy;
- Sleep disturbances, memory problems, poor appetite;
- Decreased immunity;
- The desire to hurt yourself or loved ones (including a baby);
- Hypochondria (searching for symptoms of non-existent diseases);
- Muscle pain;
- Attacks of sadness, inability to experience pleasure;
- Loss of initiative, passivity.
Signs and symptoms of postpartum depression can appear for a long time and be clearly noticeable, or the process occurs unnoticed by others (if the woman is not used to showing her weakness). The count can go on for months, and even years. If the signs of postpartum depression take on a permanent form, then the young mother needs to pay attention to her condition and seek support from those around her.
Symptoms of postpartum depression worsen quality of life, and neglected conditions can cause tragedy. Sometimes it happens that women, being in an altered state of consciousness, cause harm to newborns. Sometimes they even cause injuries incompatible with life. Close people need to show care and attention and provide all possible assistance, especially if the baby is restless. The nervous system of a woman who has recently given birth is fragile and may not be able to withstand the load that has fallen on it.
What are the causes of postpartum depression?
An important question that concerns both women themselves and their relatives: why does postpartum depression occur? Causes of postpartum depression in women:
✔️ Changes in hormonal background. During childbirth, a woman receives a shock dose of natural doping (progesterone, oxytocin and estrogen), and then the same sharp decline occurs. At the same time, the blood volume decreases overnight, the metabolic rate changes, and the vestibular apparatus is affected. All this has an impact on the body and psyche.
✔️ Dissatisfaction with your image (looks bad).
✔️ Difficult living conditions, dysfunctional family situation.
✔️ Lack of vitamins and iron deficiency (anemia) can become a provoking factor that triggers depression.
✔️ Sleep deficiency, increased physical activity, lack of help.
✔️ Restless baby.
✔️ Tendency to mental disorders, their presence in the past.
✔️ Predisposition to hysterical manifestations and depressed mood.
Postpartum syndrome in women may not manifest itself as a bad and depressed mood, but changes in the brain nevertheless occur. Depression after childbirth does not occur in everyone and occurs in different forms, but still many young mothers are at risk.
Causes of depression after childbirth
In recent years, depression that is associated with the female reproductive period has been identified as a separate category. The formation, establishment of the reproductive function and its reverse development represent a continuous life chain with critical periods of restructuring of the hormonal system and the entire organism as a whole.
The development of depression in previous links is a predisposing factor for its relapse in subsequent links in the chain. Thus, mental disorders associated with the menstrual cycle can manifest or worsen in the premenstrual period, during pregnancy or after childbirth, during natural or artificially induced menopause, and in the postmenopausal period.
For a long time, mental disorders were associated mainly with rapid hormonal changes in a woman’s body during these periods, especially in the body of a postpartum woman (a rapid decrease in the concentration of sex hormones and thyroid hormones in the blood). However, as a result of multiple studies, this assumption was not confirmed.
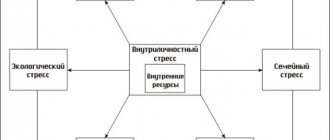
Currently, it is believed that the causes of postpartum depression lie not only in crisis biological (hormonal) changes. The mechanism of development of this disease is considered on the basis of the so-called biopsychosocial approach, that is, a complex combination of biological factors with negative psychological, socio-economic and everyday factors.
At the same time, the realization of the pathological influence of social factors occurs not directly, but indirectly - through the personal characteristics of each individual woman through a system of relationships that have special meaning for her.
An example would be chronic stress against a background of low compensatory capabilities. It can arise as a result of obstacles (the birth of a child) in the way of a woman’s fulfillment of social needs that are of high importance to her. This approach is especially important for psychotherapeutic doctors and clinical psychologists.
Multiple causes and factors that contribute to the development of pathology can be grouped into 4 groups:
- Physiological and physical causative factors arising in connection with the characteristics of changes in the body during pregnancy, the postpartum period, etc.
- Anamnestic data on predisposition to depression.
- Social reasons - family characteristics and the specifics of the social environment.
- Factors of a psychological nature - personal characteristics, perception of oneself as a mother, woman, etc.
First group
The first group of factors includes dysfunction (usually hypofunction) of the thyroid gland, a sharp decrease in the content of progesterone and estrogen in the blood after childbirth, which leads to a change in the emotional state, the appearance of lethargy, sharp mood swings from unreasonable depression to irritability, from apathy to excess energy . These changes are identical to premenstrual syndrome and menopausal disorders.
The reasons may also be changes in the intensity of metabolic processes, a decrease in circulating blood volume, severe anemia in the postpartum period, condition after cesarean section and complications during and after childbirth. And also, the presence of obstetric, gynecological and endocrine diseases, severe pain during childbirth and their stressful perception, the occurrence of problems associated with child care (lactation and breastfeeding, insufficient and restless sleep, etc.).
Physical factors include physical fatigue, a woman’s perception of her appearance after pregnancy and childbirth - changes in the shape and shape of the abdomen, temporary loss of skin elasticity, slight swelling of the face and pallor, swelling of the eyelids and “bruises” under the eyes, etc.
Factors of the second group
Considered to be high risk causes. They can be determined based on medical history and as a result of clinical monitoring of the course of pregnancy.
These include severe premenstrual syndrome, alcohol abuse, the presence of a hereditary predisposition to affective disorders (mood disorders), depression, and mental pathology. In addition, depression after a second birth may be due to the negative experience a woman acquired as a result of her previous birth.
In all these cases, pregnancy and childbirth are only a moment that provokes depression. Some of these factors can be detected in a woman already during pregnancy in the form of increased fatigue and severe emotional instability - little motivated or even unmotivated tearfulness, sudden bouts of irritability, manifestations of feelings of hopelessness and emptiness.
Social reasons (third group)
They are very numerous, varied and individual for each mother. The main ones include the lack of positive experience in family life, changes in the family’s way of life that developed before the birth of the child, intra-family disunity and difficulties in relationships with the husband and relatives, their insufficient attention or refusal of physical and moral support in caring for the child, lack of social security.
Very important in the development of postpartum depression are:
- incorrect behavior and misunderstanding on the part of the husband;
- financial and material dependence on parents or relatives;
- cessation of career growth;
- a certain isolation from the usual social circle, a change in place of residence or poor living conditions;
- loss of loved ones;
- incorrect, inattentive or rude attitude of medical workers;
- the desire of the postpartum woman to maintain maternal ideals generally accepted in society.
Psychological factors (fourth group)
If it is possible to provide a woman with optimal social and physical conditions for the birth and care of a child, then, in contrast, changing the basic psychological (personal) factors is impossible.
The main psychological factors that contribute to the formation of postpartum depressive syndrome include:
- emotional instability, increased anxiety, infantilism;
- low degree of resistance to stressful situations;
- suspiciousness and tendency to a hypochondriacal state;
- low degree of self-esteem and lack of confidence in one’s capabilities, as well as a tendency to self-blame;
- easy suggestibility, dependence and high psychological sensitivity;
- a negative type of thinking, expressed in a negative assessment of most events occurring around oneself in relation to oneself;
- tendency to depression and self-hypnosis of pathological fears (phobias);
- the type of woman’s perception of herself as a mother, depending on which maternal orientation is divided into helping and regulating. The first is characterized by a woman’s perception of motherhood as the highest degree of femininity and self-realization. The second task is to regulate the behavior of your child and treat him and household chores associated with the child as a threat to the realization of his desires. The discrepancy between orientation and opportunities for their implementation leads to a state of depression.
Manifestations of mental disorders in men
Postpartum depression in men is 2 times less common than in women, but most often it goes unnoticed. This is due to the absence of exclusively female problems in men - social, psychological, family, related to domestic discrimination, the menstrual cycle, infertility, etc.
Its causes in men are significant changes in the existing lifestyle and family relationships. For example, if previously they were accustomed to attention from their wife, relative freedom of action, interesting pastime, etc., then after the birth of a child everything depends on the newborn’s regime, the need to help the wife, allocating time for activities with the baby, sexual relationships, increased financial demands of the family arise, etc.
The man begins to feel that his wife pays little attention to him, he becomes demanding, irritable and aggressive, and withdraws into himself. Mild sedatives for postpartum depression in a man sometimes help eliminate feelings of anxiety and restlessness, but often the advice of a psychologist is more effective, both for the man and for his wife, as well as the help and attentive attitude of parents, relatives and close friends.
In the International Classification of Diseases (ICD-10), 10th revision, postpartum depressive states (depending on the causes) are distinguished as:
- current depressive episode;
- recurrent (repeated) psychopathological disorder, determined on the basis of anamnestic data;
- psychotic and behavioral disorders not classified in other categories that are associated with the postpartum period.
Why is postpartum depression dangerous?
Unfortunately, many people miss an important point and do not think about how postpartum depression affects health. Any mental problems can be dangerous for the patient and others. Losing control over yourself can end in tragedy. The consequences of postpartum depression can even manifest themselves in the form of suicide, and often the mother leaves this world with the child.
Some women fall into a difficult mental state, unable to cope with everyday difficulties combined with hormonal imbalance and severe physical fatigue. These factors can lead to a state of passion, clouding of reason and loss of control over one’s actions. At such moments, it is very important to have someone who can tell you how to cope with this condition.
Prolonged postpartum depression has a bad effect not only on the woman, but also on her child. He begins to lag behind in development, acquires neurological problems, gets sick more often and is more vulnerable. The negative impact of the disease on the health of the child and mother should be minimized through the joint efforts of the people around them. A universal recipe has not yet been invented or a magic pill has been created to overcome the syndrome, but the onset of depression can be prevented long before childbirth.
How to cope with postpartum depression?
Read how to cope with depression yourself by clicking on the link